
PSEUDORADICULAR LOWER BACK PAIN
Radicular and pseudoradicular lower back pain are different types of pain that radiate distally at the legs. Radicular pain radiates below the knee and is thought to stem from disorders associated with nerve root compression which is often felt in distal dermatomes below the knee (projected pain). In contrast, pseudoradicular pain does not radiate below the knee and is thought to be associated with local proximal disorders that do not affect any nerves or nerve roots.
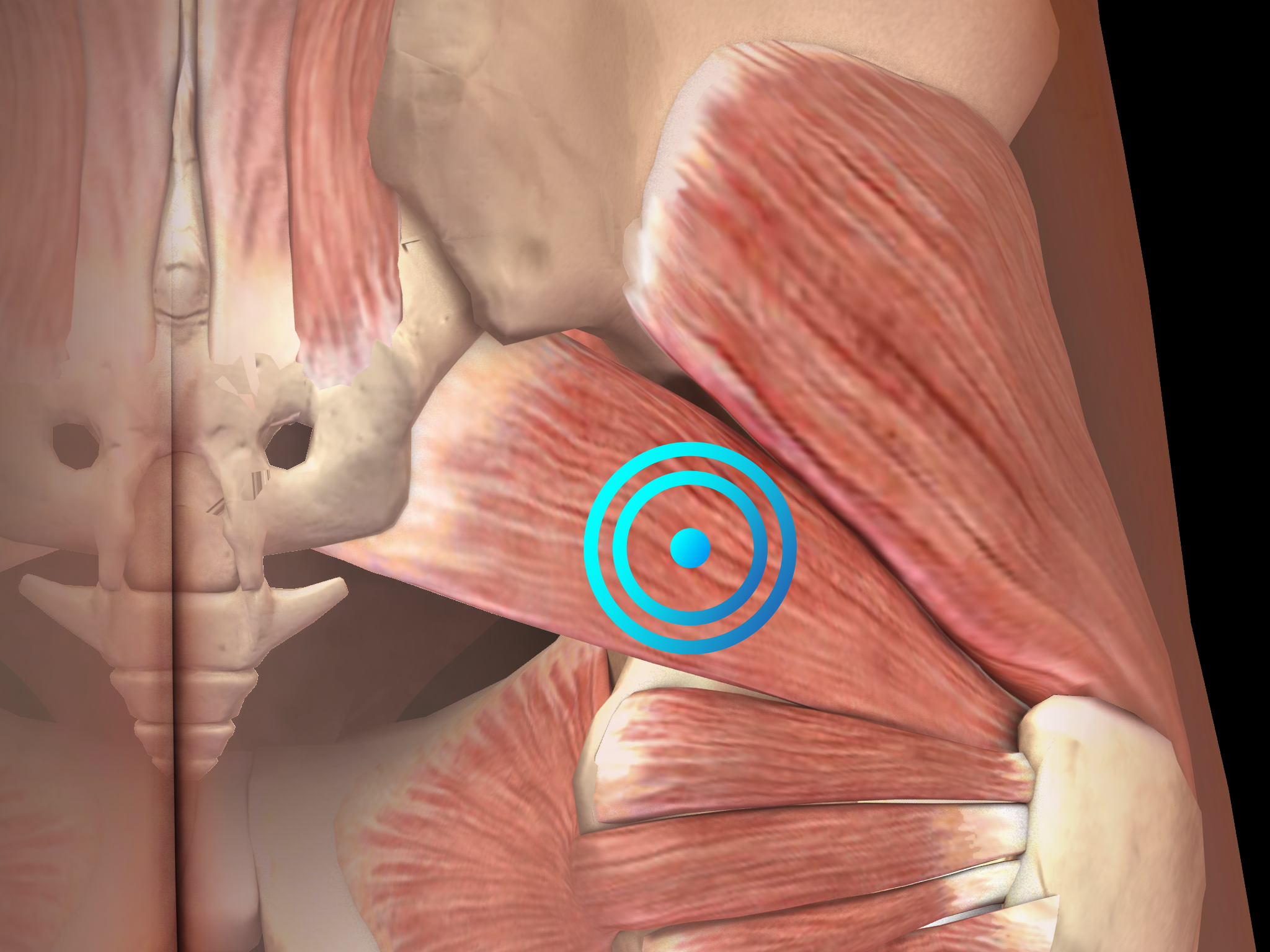
Pathology
These disorders include facet joint affection, piriformis syndrome and several other conditions. The associated pain is perceived in proximal dermatomes within the thigh (referred pain, head zones). In many cases of pseudoradicular lower back pain, it is impossible to find the underlying disease characterizing these cases as idiopathic.
The distinction between radicular and pseudoradicular lower back pain is clinically relevant for several reasons:
- Radicular pain has always a neuropathic component because it always involves damage or irritation of peripheral nerves or nerve roots. In contrast, pseudoradicular pain may occur without damage or irritation of peripheral nerves or nerve roots and, thus, might be purely nociceptive. This distinction is very important when evaluating the results of neurophysiologic examinations.
- Radicular pain (neuropathic pain) is predominantly sensitive to antidepressants and anticonvulsants. In contrast, pseudoradicular pain (nociceptive pain) is predominantly sensitive to nonsteroidal anti-inflammatory drugs (NSAIDs).
Diagnosis is based on clinical features. Diagnostic imaging should be considered to rule out other causes of lower back pain or to establish the diagnosis of radicular or pseudoradicular lower back pain when in doubt. However, it should be noted that abnormalities found in radiological examinations in the lumbar spine poorly correlate with clinical symptoms.
Radial shock wave therapy is a very effective alternative for pseudoradicular lower back pain treatment.
Side effects of Radial Shock Wave Therapy (RSWT) using the Swiss DolorClast®
When performed properly, RSWT with the Swiss DolorClast® has only minimal risks. Typical device-related non-serious adverse events are:
- Pain and discomfort during and after treatment (anaesthesia is not necessary)
- Reddening of the skin
- Petechia
- Swelling and numbness of the skin over the treatment area
These device-related non-serious adverse events usually disappear within 36h after the treatment.
Treatment Procedure
Clinical Proof
Stosswellentherapie beim idiopathischen Rückenschmerz pseudoradikulären Syndromen
Bauermeister W.
Maier m, Gillesberger F: Abstract 2003 zur Muskuloskelettalen Stosswellentherapie: Norderstedt, 2003, 29-34
This article shows how shock wave therapy can be used to treat idiopathic back pain pseudoradicular syndromes.
(German Study)
Recommended Settings
| Recommended Settings | Treatment |
| Number of treatment sessions | 3 to 5 |
| Interval between two sessions | 1 week |
| Air pressure Evo Blue® | 2 to 4 bar |
| Air pressure Power+ | 1.5 to 3 bar |
| Impulses | 500 - 1000 impulses per trigger point |
| Frequency | 12Hz |
| Applicator | 15mm or 15 mm trigger |
| Skin pressure | Light to Moderate |
Contraindications
The following contraindications of RSWT using the Swiss DolorClast® must be considered:
- Treatment over air-filled tissue (lung, gut)
- Treatment of pre-ruptured tendons
- Treatment of pregnant women
- Treatment of patients under the age of 18 years (except for Osgood-Schlatter disease and muscular dysfunction in children with spastic movement disorders)
- Treatment of patients with blood-clotting disorders (including local thrombosis)
- Treatment of patients treated with oral anticoagulants
- Treatment of tissue with local tumors or local bacterial and/or viral infections
- Treatment of patients treated with cortisone
Some indications may not be approved in the United States of America, under regulation by the US FDA. Please refer to the respective Instructions for Use.
